Overview
Modalities are combined to create a treatment program that is appropriate for the patient and is based on patient and tumor characteristics as well as patient preferences.
Treatment of cancer can involve any of several modalities:
Radiation Therapy:
Radiation treatment or radiotherapy is the use of precisely calculated doses of high-energy X-rays to treat parts of the body where there is cancer. It is generally a pain-free treatment and external radiation therapy does not cause you to be radioactive.
Chemotherapy:
Chemotherapy is the use of drugs to destroy rapidly growing cancer cells. Some kinds of chemotherapy may slow the growth of cancer cells, and keep them from spreading to other parts of the body. It may be used with radiation to help shrink the tumor before surgery. It may also be used after surgery or radiation to destroy remnant cancer cells. At the center, chemotherapy is given as an outpatient procedure at our specialized treatment areas, managed by a team of oncology-trained nurses who provide close monitoring.
Surgery:
Surgery plays a pivotal role in the management of most solid cancer. While surgery alone is adequate for early cancers, most advanced tumors require multi-modality treatment.
Radiation Oncology
Infinity with Agility - Linear Accelarator
We have consistently brought cutting-edge technology to our patients, Elekta Infinity with Agility™ first in India.
The Infinity with Agility- linear accelerator enables extremely accurate, image-guided adaptive radiotherapy to be delivered safely and in a short period of time. This makes it possible to irradiate any site in the body with great precision. Agility, a multi-leaf facilitates faster and more accurate delivery of radiotherapy. Agility offers high-resolution beam shaping capabilities including inter digitation across the 40×40 cm field size.
Volumetric Modulated Arc Therapy (VMAT/Rotational IMRT)
VMAT is a novel radiation technique, which can achieve highly conformal dose distributions with improved target volume coverage and sparing of normal tissues compared with conventional radiotherapy techniques. VMAT also has the potential to offer additional advantages, such as reduced treatment delivery time compared with conventional static field intensity-modulated radiotherapy (IMRT).
Stereotactic Body Radiotherapy (SBRT)
SBRT is also called stereotactic ablative radiotherapy (SABR), is a type of radiation therapy in which a few very high doses of radiation are delivered to small, well-defined tumors. The goal is to deliver a radiation dose that is high enough to kill cancer while minimizing exposure to surrounding healthy organs. Stereotactic radiation treatment for the body means that a specially designed coordinate system is used for the exact localization of the tumors in the body in order to treat them with limited but highly precise treatment fields. SBRT involves the delivery of a single high dose radiation treatment or a few fractionated radiation treatments
Image-Guided Radiotherapy (IGRT )
IGRT is a step forward of IMRT in which various biological and anatomical imaging techniques are integrated into the radiation therapy process. The overall goal of IGRT is to target tumors more accurately while better sparing the normal tissues. Our machine has an onboard CT scanner with VK imaging facility capable of online and offline matching of the planned image with treatment image accurately.
Intensity Modulated Radiotherapy (IMRT)
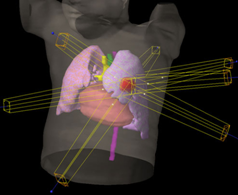
This is a specialized form of 3 D conformal radiotherapy. As the name implies, intensity-modulated radiation allows us to modulate the intensity of each radiation beam which is divided into thousands of beamlets, so each field may have one or many areas of high-intensity radiation and any number of lower intensity areas within the same field, thus allowing for greater control of the dose distribution with the target. This achieves maximum dose envelop to the tumor sparing the surrounding normal structures.
Stereotactic Radiotherapy (SRT)/(SRS)
SRT is a specialized type of external beam radiation therapy that uses focused radiation beams targeting a well-defined tumor, relying on detailed imaging, computerized three-dimensional treatment planning, and precise treatment set up to deliver the radiation dose with extreme accuracy.
Three-dimensional Conformal Radiation Therapy (3D CRT)
3D CRT is a technique where the beams of radiation used in the treatment are shaped to match the tumor. Conformal radiation therapy uses the targeting information to focus precisely on the tumor while avoiding the healthy surrounding tissue.
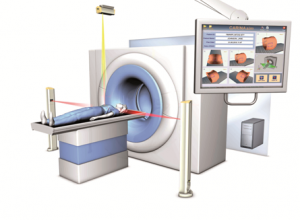
CT Simulator
CT simulation transmits X-rays through the tissue to create a graphic display of the tumor and surrounding normal tissues. The simulator allows for precise treatment planning by demonstrating the relationship between the target tumor and healthy tissues while the patient is in the treatment position.
Specially designed for the specific needs of radiation therapy planning for advanced treatment methods such as conformal, IMRT, or stereotactic radiotherapy. The large bore of 80cm, moving lasers and the accurate table alignment allow for highly precise patient positioning.
Using Siemens’ z-Sharp technology the SOMATOM Definition AS can provide the fastest sub-millimeter volume coverage at the industry’s highest spatial resolution, preparing optimally for advanced treatment techniques such as SRS and SBRT
Additionally, its large bore of 80 cm and a table load capacity of up to 307 kg opens this CT to all patients, meaning that virtually no patient is excluded and even clinically challenging cases like in the ED or bariatric patients can be imaged rapidly from head to toe without difficulty.
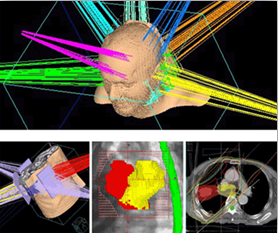
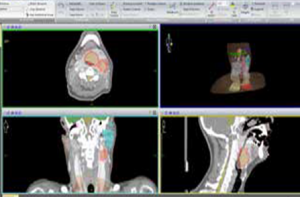
Treatment Planning System (TPS)
MONACO is presently the only planning system that uses super accurate and complex Monte Carlo Dose engine algorithm in the Dose calculation. This is considered the "gold standard" in planning. MONACO also allows biological based Dose modelling, which ensures that doses receiving to the normal structures are kept well below their tolerance limit. ONCENTRA and Multimodality Work Place (MMWP) for planning, contouring and image fusion to streamline the complex treatments planning process.
.jpg)

Brachytherapy
AIMS Hospital offers a comprehensive cancer care program, including advanced treatments like High-dose Rate (HDR) brachytherapy. Best of all, you’ll appreciate convenient appointment times, a location near you, and a personalized focus to meet your needs before, during, and after your procedure.
What is Brachytherapy?
Brachytherapy is a well-established form of internal radiation therapy that uses radioactive sources positioned directly into or around the tumor. Brachytherapy (from the Greek: brachy = short) works in a different way.
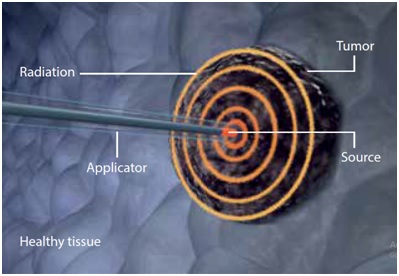
In comparison to External Beam Radiation Therapy (EBRT), brachytherapy delivers a higher dose of radiation to specific sites in the body because this technique targets the tumor and minimizes radiation to the surrounding healthy tissue (Figure 1). For the patient, this means shorter treatment periods, fewer side effects, and a faster recovery.
Fig 1: Localized radiation to tumor cells via brachytherapy
Most HDR brachytherapy treatments are done with one weekly treatment for a period of up to four weeks or with one or two treatments per day for up to five days. These common indications may differ in some cases. The radiation delivery only lasts a few minutes while the procedure (also called a session) including patient setup, applicator positioning, treatment planning, and treatment delivery itself, lasts up to a few hours.

HDR Brachytherapy for Breast Cancer
The most common treatment for breast cancer is surgery either with partial removal of the breast tissue where the tumor is located (lumpectomy) or complete removal of the breast (mastectomy). The surgery is often combined with radiation treatment.
One of the most promising and efficient radiation treatment options for breast cancer, today, is HDR brachytherapy (Figure 2). There are three types of breast cancer patients who qualify for HDR brachytherapy:
- Those who have early-stage breast cancer.
- Those who have locally advanced breast disease, but no metastasis.
- Those who have recurrent breast cancer to the chest wall (these patients may not be candidates for surgery or choose not to have surgery).
HDR brachytherapy was developed to reduce the risk of recurrence while shortening the amount of time it takes to complete the radiation treatment.
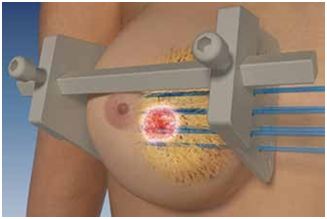
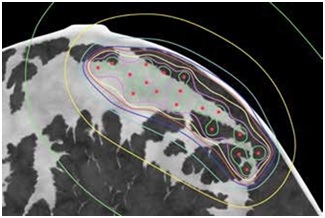
Fig 2: Placement of catheters in the breast for interstitial HDR using a special template
Fig: CT Image showing the position and intensity of the dose distribution in the breast
With a few well-placed catheters, HDR brachytherapy can provide a targeted treatment. If high-dose radiotherapy is used, it typically requires one to two treatments per day for about one week. Each treatment session will last about one hour. However, during the treatment, the radioactive source is inside your breast for only a few minutes. Once the course of the treatment is completed, the catheters are removed.
As compared to EBRT, the most important advantages of HDR brachytherapy are:
- Overall treatment time is one week versus six to seven weeks for EBRT.
- Yields excellent cosmetic results.
- It delivers a precise, highly concentrated dose of radiation directly to the tumor bed, for a short time.
- Reduces radiation dose and possible damage to adjacent organs such as the opposite breast and the lungs.
- Very low risk of cancer recurrence.
HDR Brachytherapy for Gynaecological Cancer
For endometrial and cervical cancer, HDR brachytherapy is delivered using special intra-vaginal applicators for the introduction of the radioactive source (Figure 3). Once the treatment is done, the applicator is removed and the patient can continue her day. Patients with cervical cancer will require a few short treatments given over a couple of days.
For vaginal cancer, a cylinder similar to a plastic tampon with a central channel is used. After placement of the cylinder, it is connected to the HDR after loader where the radioactive source is stored until the time of treatment. After the treatment is complete, the vaginal cylinder is disconnected and removed from the patient. The treatment takes about an hour and most patients will require only a few treatment sessions. After the treatment is complete, the patient can continue with her day as this type of treatment is extremely well-tolerated.
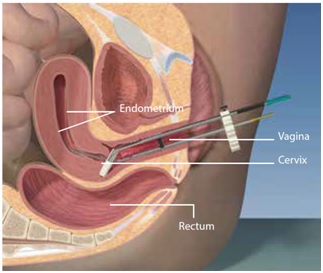
Fig 3: Intra-vaginal applicator for HDR brachytherapy
The benefits of HDR brachytherapy in the treatment of gynecological cancers are:
- High-dose precisely targeted to the tumor with minimal exposure to adjacent tissues and organs. The risk of radiation to the rectum and bladder is minimized by the precision delivery of the radiation dose.
- Treatment can be delivered on an outpatient basis within a few days.
- Short treatment and recovery times provide convenience to patients.
- Few side effects and complications as compared to other radiation procedures.
Recovery after Brachytherapy
Most people undergoing HDR brachytherapy can return home after treatment. In most cases, you can return to normal activities right away.

Brain Cancer
A brain tumor is a cancerous/non-cancerous mass or growth of abnormal cells in the brain. Two of the most common forms of brain cancer are Metastatic Brain Tumors (secondary spread from other parts) and Glioma (primarily from the brain).
Warning signs
- Headaches (usually worse in the morning)
- Vomiting
- Muscle jerking or twitching (seizures or convulsions)
- Vision problem
- Speech & Hearing difficulty
- Weakness in the arms & legs
- Changes in mood, personality, or ability to concentrate
- Numbness or tingling in the arms or legs
- Memory loss
Risk factors
- Radiation exposure
- Family history
- Immune system disorders
- Environmental factors such as exposure to vinyl chloride (a chemical used to manufacture plastics), petroleum products, etc
Progression
Malignant primary brain tumors are cancers that originate in the brain, typically grow faster than benign tumors, and aggressively invade surrounding tissue. Although brain cancer rarely spreads to other organs, it will spread to other parts of the brain and the central nervous system.
Diagnosis
Primary diagnosis:
Physical exam and personal/family health history
Advanced diagnosis:
Neurologic exam, MRI, CT Scan, Angiogram and Biopsy
The mainstay of diagnosis is currently an MRI scan followed by surgery for histological examination by a pathologist.
Treatment in a nutshell:
The standard treatment for brain tumors includes surgery, radiation therapy, and/or chemotherapy. In general, radiation and chemotherapy treatments are used as secondary or adjuvant treatments for malignant tumors. However, radiation and chemotherapy may be used without surgery if the tumor is inoperable.
Cancer Oesophagus
The Oesophagus is a tube that starts in the neck, traverses through the chest, and joins the stomach in the upper abdomen. It transports food from the mouth into the stomach. In cancer of the oesophagus (food pipe), a malignant (cancerous) tumor arises in the innermost lining of the tube. It then progresses outwards, lengthwise, and circumferentially to cause progressively increasing difficulty in swallowing. The two most common forms of cancer oesophagus are squamous cell carcinoma and adenocarcinoma; the latter generally involved the lower part of the oesophagus near the stomach.
Tobacco and heavy alcohol use are known to increase the risk of developing cancer of the oesophagus. People with long-standing reflux disease and anemia (women in particular) also have an increased risk of developing cancer of the oesophagus.
Warning signs
- Difficulty in swallowing/ painful swallowing
- Weight loss
- Pain behind the breastbone
- Hoarseness and cough
- Indigestion and heartburn
- Black stools or blood in vomit
- Long-standing reflux (acidity)
Risk factors
- Tobacco, alcohol, and tambul (betel nut)
- Gastroesophageal reflux disease (GERD)
- Obesity
- Exposure to chemical fumes
- Injury to oesophagus
Progression
- Stage 0: Cancer is confined to the lining of the oesophagus
- Stage 1: Cancer has spread deeper into the tissues of the oesophagus
- Stage 2: Cancer may now affect lymph nodes near the oesophagus
- Stage 3: Cancer has progressed to surrounding tissues
- Stage 4: Cancer has metastasized, or spread, to other parts of the body
Diagnosis
- Primary diagnosis: Physical examination
- Secondary diagnosis: Barium swallow, Oesophago-Gastro-Duodenoscopy, CT Scan with contrast, PET CT scan whole body
The following tests and procedures are necessary for confirming the diagnosis:
- Barium Swallow: A series of x – rays of the esophagus and stomach. The patient drinks a liquid that contains barium (a silver-white metallic compound). The liquid coats the esophagus and an x-ray is taken
- Oesophago-Gastro-Duodenoscopy: This involves introducing a flexible telescope through the mouth to visualize the esophagus and stomach. A biopsy may be done at the same time if the tumor is seen at endoscopy
- CT Scan with Contrast: This is computerized imaging of the chest and abdomen did after intravenous and oral contrast. This gives information about the location, extent, and spread of spread disease and hence helps in planning treatment
- PET CT Scan Whole Body: This is a combination of CT scans of the entire body and PET. It involves giving a special dye before scanning. The dye (FDG) helps in identifying the spread of disease and thus is more accurate for the staging of disease and planning of treatment. The treatment depends on the stage of cancer. Cancer of the esophagus is staged from I to IV; stage I is early, localized cancer and stage IV is when cancer has spread to other organs such as lung, liver bone, etc., or neighboring structures, such as a tracheobronchial tree, nerves, or aorta.
Colorectal Cancer
For most people, a tummy ache is just that. A simple tummy ache is something we tend to take very casually. But, on occasion, a stomach ache can be indicative of a far more serious problem – digestive tract complications, colitis, and even cancer. Tackling these conditions at an early stage ensures you a better chance of survival. In cases involving colonic cancer and colitis, timely intervention can save the lives of 70-80% of patients. So, make it a point to visit your doctor regularly for check-ups.
Colorectal cancer starts in the colon or the rectum. These cancers can also be named colon cancer or rectal cancer, depending on where they start.
Warning signs
- Persistent constipation or diarrhea
- An urgency to move the bowels
- Rectal cramping, or rectal bleeding
- Dark patches of blood in or on a stool; or long, thin, “pencil stools”
- Abdominal discomfort or bloating
- Unexplained fatigue, loss of appetite, and/or weight loss
- Pelvic pain, which occurs at later stages of the disease
Risk factors
- Older age (after 50)
- Inflammatory bowel disease, Crohn’s disease, or ulcerative colitis
- A personal or family history of colorectal cancer or colorectal polyps
- Lack of regular physical activity
- Low fruit and vegetable intake
- A low-fiber and high-fat diet
- Overweight and obesity
- Alcohol consumption
- Tobacco use
Progression
- Stage I: Cancer has grown through the mucosa and has invaded the muscular layer of the colon or rectum.
- Stage II: Cancer has grown through the wall of the colon or rectum
- Stage III: Cancer has grown through the inner lining or into the muscle layers of the intestine and spread to one to three lymph nodes
- Stage IV: Cancer has spread to different organs like lungs, bones, liver, lymph nodes, brain, or spinal cord.
Diagnosis:
- Primary diagnosis: Physical examination, blood tests
- Advanced diagnosis: Colonoscopy (using a scope to examine the inside of your colon).
Gall Bladder Cancer
Most gall bladder cancers start in the glandular cells in the gall bladder. The gallbladder is a small, pear-shaped organ under the liver. The gallbladder concentrates and stores bile, a fluid made in the liver.
Warning signs
- Nausea & Vomiting
- Lump in abdomen
- Abdominal bloating
- Upper abdominal pain
- Fever
- Weight loss
- Jaundice
Risk factors
- Gallstones
- Porcelain gallbladder (incidence higher in females of Northern India)
- Obesity
- Older age
- Choledochal cysts
- Gallbladder polyps
- Primary sclerosing cholangitis
- Industrial and environmental chemicals
- Typhoid and family history
Progression
The tumor which is present as a small gallbladder mass may spread to the liver, bile duct, vessels, or adjacent organ and can present as a mass in the abdomen, jaundice, fluid in the tummy, vomiting, cachexia.
Diagnosis
Tests such as Biopsy, X-ray, Percutaneous cholangiography, Blood tests, Computed tomography (CT or CAT) scan, Magnetic resonance imaging (MRI). Clinical symptoms along with biochemical tests and tumor markers (CA 19-9, CEA) are used for diagnosis. A biopsy is carried out only for inoperable cases (for palliative therapy).
Gynecological Oncology
Gynecologic oncology is a subspecialty of Obstetrics and Gynecology that focuses on diagnosing and treating women with cancers of the reproductive system. Cancers can occur in any part of the female reproductive system—the vulva, vagina, cervix, uterus, fallopian tubes, or ovaries. These cancers are called gynecologic cancers. Each woman with gynecological cancer has unique medical and emotional needs. To meet these needs, AIMS hospital has highly qualified experts who are specialized in different modalities of cancer care and work as a team, backed by cutting-edge technology.
Aim of Gynecologic Oncology services at AIMS Hospital
- To provide high quality, evidence-based comprehensive, and personalized care to patients with a suspected or diagnosed Gynecological cancer
- To coordinate with social organizations in order to increase awareness of the general public about Gynecological cancer screening, prevention, and early detection
- To participate in national and international research in the field of Gynecological Oncology that will reduce the incidence of gynecologic cancer and improve the survival and quality of life of patients with gynecologic cancer
- To offer services with the help of a multidisciplinary team from prevention to palliation
The spectrum of diseases treated by the Gynecological Oncology unit
- Premalignant Diseases of Vulva and Vagina
- Premalignant Diseases of Cervix
- Cervical Cancer
- Endometrial Cancer
- Ovarian Cancer
- Vulval Cancer
- Vaginal Cancer
- Cancer of Fallopian Tube
- Gestational TrophoblsaticNeoplasia
Services provided by the Gynecological Oncology unit
The Gynecological Oncology services provide a full range of women’s health care, including Diagnostic, Consultative, and Treatment services. Following services are offered by our Gynecological Oncology unit.
- Screening for Cervical Cancer: Pap Smear/Liquid-based cytology/ HPV testing
- Colposcopy Clinic
- Excision Procedures for Premalignant Lesions of Cervix: (Loop Electro-surgical Excision/ Cone Biopsy)
- Evaluation/consultation and Counseling for high-risk individuals due to strong family history of Ovarian/Breast Cancers
- Surgical procedures for diagnosed cases of Gynecological Cancers –
- Surgery for early Ovarian Cancer (Staging Laparotomy)
- Surgery for advanced Ovarian Cancer (Debulking Surgery)
- Radical Hysterectomy (Wertheim’s Operation )
- Surgery for Endometrial Cancer
- Total Pelvic Exentration
- Anterior/Posterior Pelvic Exentration
- Pelvic/Paraortic (Retroperitoneal) Lymph Node Dissection
- Radical Vulvectomy + Groin Node Dissection
- Radical Vulvectomy + Reconstruction.
Head & Neck Cancer
 Head and neck cancers are cancers that start in the tissues and organs of the head and neck. They include cancers of the larynx (voice box), throat, lips, mouth, nose, and salivary glands. Most types of head and neck cancer begin in squamous cells that line the moist surfaces inside the head and neck (for example, the mouth, nose, and throat).
Head and neck cancers are cancers that start in the tissues and organs of the head and neck. They include cancers of the larynx (voice box), throat, lips, mouth, nose, and salivary glands. Most types of head and neck cancer begin in squamous cells that line the moist surfaces inside the head and neck (for example, the mouth, nose, and throat).
Cancer of the head and neck are the most common cancers in India (30% of all cancers). Gone are the days when a stand-alone surgeon could treat a patient of head and neck cancer. Treatment of head and neck cancer now requires a multi-disciplinary approach with a team comprising of a head and neck cancer surgeon, a reconstructive surgeon, an onco-anaesthetist, a radiation oncologist, a medical oncologist, an onco-pathologist, a speech and swallowing therapist, a physiotherapist, a dental surgeon, an occupational therapist and a medical counselor.
In the past, the treatment of head and neck cancer was only aimed at cancer-free survival. Issues like cosmoses, speech, swallowing, pain relief etc. were considered secondary. Over the last few years, the goals of such treatments have changed. Now, in addition to improved survival, we also aim to improve the quality of life of our patients with better cosmoses, better functional outcomes like normal speech, swallowing, taste, smell etc. Each member of the multi-disciplinary team works towards the goal of improving the quality of life of head and neck cancer patients. And, a good team can deliver excellent service with the support of advanced infrastructure.
Warning signs
- Persistent sore throat
- Foul breath
- Hoarseness voice changes
- Swelling of throat
- Lump, bump, or mass without pain
- White or red patch, non-healthy oral ulcer
- Persistent nasal obstructions or congestions
Risk factors
Three substances greatly increase the risk of developing head and neck cancers :
- Tobacco: Tobacco in all forms like cigarettes, cigars or pipes, chewing tobacco and using snuff is harmful. Topical application in the form of masheri. The single largest factor (85 per cent) of head and neck cancers are linked to tobacco use.
- Alcohol: Frequent and heavy alcohol consumption raises the risk of developing cancers in the mouth, pharynx, larynx and oesophagus.
- Human papilloma virus, Epstein barr virus
Progression
Ahead and neck cancer can progress from the primary site to the draining lymph nodes. Hematogenous (through bloodstream) is much less common in head & neck cancers.
Diagnosis
- Primary diagnosis: Patient’s medical history, physical examination
- Secondary diagnosis: Diagnostic tests like endoscopy, lab tests, radiographs, CT scan, MRI, PET scan. Examination of the ample tissue under the microscope (mandatory to confirm a diagnosis)
- Advanced diagnosis: Once cancer is confirmed, the stage needs to be known for which examination under anesthesia (in the operating room), X-rays, and other imaging procedures like CT scan, MRI, etc. can be carried out
Treatment in a nutshell
The treatment requires a multidisciplinary approach with a team of Head and neck cancer surgeons, reconstructive surgeons, an onco-anesthetist, radiation oncologists, a medical oncologist, an onco-pathologist, a speech and swallowing therapist, a physiotherapist, a dental surgeon, an occupational therapist, and a medical counselor. In the past, the treatment was only aimed at cancer-free survival. Issues like cosmesis, speech, swallowing, and pain relief were considered secondary. Over the last few years, priority is given to improve the quality of life to our patients with better cosmesis and functional outcomes like speech, swallowing. Each member of the team works towards this goal, which is not possible without the required infrastructure.
- Surgery: During surgery, the aim is to remove the diseased tissue and get healthy margins around it to be safe. The tissue removed is sent for a Pathological evaluation which takes approximately 8 – 10 days.
- Radiation/Chemotherapy: After the report is reviewed, a call may be taken for further treatment like Radiation with or without chemotherapy. You may need further consultation with a Radiation and/or a Medical Oncologist for the same.
Additional treatment usually begins 4 – 6 weeks after your surgery.
Kidney Cancer
This is cancer that starts in the kidney. The most common type of kidney cancer is called Renal Cell Carcinoma (RCC). About 90 percent of all kidney cancers are renal cell carcinomas. The other 10 percent are made up of transitional cell carcinomas, Wilm’s tumors (found in children), and other rare tumors.
There are about 190,000 new cases of kidney cancer each year around the world, which means it accounts for about one in fifty cancers. In the UK and USA, it is about the tenth most common type of cancer. Estimated new cases and deaths from kidney (renal cell and renal pelvis) cancer in the United States in 2012: New cases: 64,770, Deaths: 13,570. Reports say even in India the incidence is increasing.
Why one needs to be aware?
Knowing the facts could save your life or the life of someone you love. Kidney Cancer is a rare cancer which does not respond to traditional chemotherapies or radiation. It is NOT something doctors typical check for. If found due to symptoms, it’s usually in the late stages. If found early, it’s usually found due to an scan/ultrasound/MRI being performed for another reason. There is always hope and the most important thing is find a doctor who specializes in renal cell carcinoma.
Do you fall in the high risk group?
- Renal cell carcinoma is the most common type of kidney cancer in adults. It occurs most often in men ages 50 – 70.
- Genetics: Genetic changes which predispose individual to probability of increased cancer risk
- Smoking: Cigarette Smokers are twice as likely as nonsmokers to develop kidney cancer. Chewing Tobacco also may increase the risk of this disease.
- Obesity
- High Blood Pressure
- Long-Term Dialysis
- Von Hippel-Lindau (VHL) Syndrome: An abnormal VHL gene increases the risk of kidney cancer. It also can cause cysts or tumors in the eyes, brain, and other parts of the bod
- Occupation: Coke oven workers in the iron and steel industry are at risk. Workers exposed to asbestos or cadmium also may be at risk
However, many people with kidney cancer have no known risk factors. On the other hand, people who have one or more known risk factors may never get the disease
What are the common signs and symptoms?
In the early stages, kidney cancer often causes no symptoms. It is usually detected by imaging like ultrasonography and CT scan of abdomen done as health check-up or for vague symptoms. As cancer grows, symptoms may develop. These are the most common symptoms in people with kidney cancer:
Warning signs
- Blood in the urine
- Side or back pain
- A mass or lump in the side or lower back
- Fatigue, which is a chronic, unexplained tiredness
- Rapid weight loss without making an effort to lose weight
- Other symptoms, such as fever with no known cause, leg or ankle swelling, and high blood pressure
Risk factors
- Age more than 40
- Smoking
- Risk is more in men than women
- Obesity
- Long-term pain medication (over-the-counter drugs and prescription drugs
- Genetic conditions like von Hippel-Lindau (VHL) disease or inherited papillary renal cell carcinoma
- Family history of kidney cancer
- Exposure to chemicals like asbestos, cadmium, benzene, organic solvents, or certain herbicides
- High blood pressure
- The risk in blacks is slightly higher than in whites.
- For an unknown reason, there is an increased risk of kidney cancer in patients with lymphoma.
Leukemia (Blood Cancer)
Leukemia is a type of cancer that affects the blood and bone marrow. Normally all blood cells are produced by the bone marrow (the spongy area in the middle of bones) in a controlled fashion. All leukemia have in the common property that the leukemia cells are abnormal and do not respond to normal control mechanisms. Large numbers of leukemia cells build up as they multiply or because they live much longer than normal cells, or both. With many leukemia cells in the bone marrow, they spill out into the bloodstream.
If you develop leukemia it is important to know exactly what type it is. This is because the outlook (prognosis) and treatments vary for the different types. know more
What are common types of Leukemia?
The four most common types of leukemia are:
- Acute Myeloid Leukemia (AML)
- Acute Lymphoblastic Leukemia (ALL)
- Chronic Myeloid Leukemia (CML)
- Chronic Lymphocytic Leukemia (CLL)
Each main type of leukemia is named according to the type of cell that is affected (a myeloid cell or a lymphoid cell) and whether the disease begins in mature or immature cells. People can get leukemia at any age. It is most common in people over age 60. The most common types in adults are AML and CLL. ALL is the most common form of leukemia in children.
What causes Leukemia?
In most cases of leukemia, the reason why a cell becomes abnormal is not known. There are certain risk factors that increase the chance that certain leukemia will develop, but these only accounts for a small number of cases. Risk factors for some types of leukemia include:
- Radiation: Previous radiotherapy for another condition. Many of the survivors of the atom bomb used in World War II developed leukemia due to the fall out of radiation
- Past treatment with chemotherapy or other drugs that weaken the immune system
- Certain genetic disorders e.g. Down’s syndrome
- Exposure to certain chemicals, such as benzene
What are the signs & symptoms of Leukemia?
As large numbers of abnormal blood cells are made, much of the bone marrow fills with these abnormal cells. Because of this, it is difficult for normal cells in the bone marrow to survive and produce enough normal mature blood cells. Also, the abnormal cells spill out into the bloodstream.
Therefore, the main problems which can develop include:
- Tiredness or no energy
- Shortness of breath during physical activity
- Pale skin
- Mild fever or night sweats
- Slow healing of cuts and excess bleeding
- Black-and-blue marks (bruises) for no clear reason
- Pinhead-size red spots under the skin
- Aches in bones or joints (for example, knees, hips, or shoulders)
- Low white cell counts, especially monocytes or neutrophils
Also, there are a reduced number of normal white blood cells which usually combat infection. Therefore, serious infections are more likely to develop. Depending on the type and site of infection which develops, the symptoms can vary greatly.
The time is taken to develop these symptoms after the disease starts varies. Typically, it is within weeks for ALL or AML. It may take months or years for symptoms to develop with CLL or CML as this leukemia progresses slowly.
Warning signs
- Pain in the bones or joints
- Swollen lymph nodes
- Fevers or night sweats
- Feeling weak or tired
- Bleeding and bruising easily
- Frequent infections
- Discomfort or swelling in the abdomen
- Weight loss/loss of appetite
Risk factors
Most cases arise without a known cause. However, some known risk factors are:
- Exposure to certain chemicals, such as benzene
- Smoking
- Certain genetic disorders, such as Down syndrome
- Certain types of previous cancer treatments like chemotherapy or radiation therapy (this happens rarely)
- Family history of blood cancer
Liver Cancer
The liver continuously filters blood that circulates through the body, converting nutrients and drugs absorbed from the digestive tract into ready-to-use chemicals. The liver can be affected by primary liver cancer, which arises in the liver, or by cancer that forms in other parts of the body and then spreads to the liver.
Warning signs
- Nausea & Vomiting
- Abdominal bloating
- Loss of appetite
- Weakness & fatigue
Some other symptoms are swelling of the abdomen (fluid in the abdomen), upper abdominal pain, itching, passing white-colored stools, etc.
Risk factors>
- Men are more likely to get hepatocellular carcinoma than women
- Obesity can increase the risk for hepatocellular carcinoma
- Studies have suggested a link between diabetes and liver cancer. This is likely due to the link between diabetes and fatty liver disease
- Diseases that disrupt the normal metabolism of the body have been shown to increase your risk of liver cancer
- Long-term alcohol use has been linked to an increased risk of liver cancer. Regular, heavy alcohol use can damage the liver, leading to inflammation. This, in turn, might raise the risk of liver cancer
- Studies have found a link between liver cancer and some rare diseases like alpha -1-antitrypsin deficiency, tyrosinemia, and Wilson’s disease, haemochromatosis
- Patients with known cirrhosis, chronic liver disease (Hepatitis B/C, ETOH related), chronic infection HBV, HCV Exposure to Aflatoxins
Progression
Primary liver tumor:
May develop new symptoms like jaundice and mass or fluid tummy from solitary to multiple, from one side to another side, or diffuse involvement of the entire liver. It spreads to lungs, bones, blood vessels, and lymph nodes.
Secondary (Metastatic) tumor
Generally, Stage IV tumors can involve the liver. The site of origin could be the GI tract or other organs (lung, thyroid, breast, biliary tract, and pancreas). Patients with chronic liver disease should undergo screening to detect tumors at an early stage.
Lung Cancer
Lung cancer, also known as lung carcinoma, is the uncontrolled growth of abnormal cells in one or both lungs. It most often occurs in people who smoke. As lung cancer grows, abnormal cells can form tumors and interfere with the functioning of the lung, which provides oxygen to the body via the blood.
Warning signs
Lung cancer is generally diagnosed on a chest X-ray, which is done for other reasons or as part of a health check-up. The associated symptoms of lung cancer include:
- Persistent cough
- Blood in sputum (spit or phlegm)
- Shortness of breath—either on exertion or at rest
- Chest pain
- Change in voice
Risk factors
- Tobacco smoking (causes 60-65 percent of lung cancers)
- Exposure to second-hand or passive smoking
- Exposure to radon gas, asbestos, and other carcinogens
- Family history of lung cancer
Progression
- Stage I: Cancer is confined to the lung
- Stage II/III: Cancer is confined to the chest
- Stage IV: Cancer spreads to other organs (lymph nodes, brain, liver, adrenal glands)
Diagnosis
Over 80 percent of lung cancers have a chance to be cured if detected early. Lung cancer is diagnosed in the following ways:
-
Primary Diagnosis: Chest X-ray or a CT scan
-
Secondary diagnosis: Bronchoscopy, EBUS (Endobronchial Ultrasound), or CT-guided biopsy for obtaining tissue from the tumor
-
Advanced Diagnosis: PET CT whole body, MRI, Mediastinoscopy, and other surgical procedures.
Lymphoma
Lymphoma is a cancer of lymphatic cells in the lymphatic system. About 54 percent of the blood cancers that occur each year are types of lymphoma. Lymphomas are divided into two types – Hodgkin’s lymphoma and non-Hodgkin’s lymphoma. There are various types of non-Hodgkin’s lymphoma which are divided into high-grade (fast-growing) and low-grade (slow-growing). It is important to know exactly what type you have. This is because the treatments and outlook (prognosis) can vary for different types of lymphoma. The majority of lymphoma can be cured with treatment.
What is the lymphatic system?
The lymphatic system consists of lymph nodes (glands), a network of thin lymphatic channels (like thin blood vessels), and organs, such as the spleen and thymus.
The lymphatic system also forms a major part of the immune system. Lymph and lymph nodes contain white blood cells called lymphocytes and antibodies which defend the body against infection. The lymphocytes are made in the bone marrow. When they are mature they are released into the bloodstream and migrate into the lymphatic system.
There are three types of mature lymphocytes:
- B lymphocytes make antibodies that attack infecting bacteria, viruses, etc.
- T lymphocytes (which finish off their maturing in the thymus gland) have various functions, including helping the B lymphocytes to make antibodies.
- Natural killer lymphocytes also help to protect against infection.
What causes a Lymphoma and how does it develop?
The exact cause is not known. If your immune system is down (for example, if you have AIDS) your risk of developing lymphoma is increased. Previous infection with a virus called the Epstein-Barr virus, HTLV may increase the risk slightly. However, many people have an infection with the Epstein-Barr virus, and the vast majority do not develop Hodgkin’s lymphoma. However, this only accounts for a small number of cases, and the cause are unknown for most people. It is not an inherited condition and does not run in families.
The origin of cancer (such as lymphoma) starts from one abnormal cell. Exactly why the cell becomes cancerous is unclear. It is believed to be something that damages or alters certain genes in the cell making the cell abnormal. These cells multiply and produce many more abnormal cells. The cancerous lymphocytes tend to collect in lymph nodes. The lymph nodes become bigger and form cancerous tumors. Some abnormal cells may travel to other parts of the lymphatic system, such as the spleen. So you may develop lots of large cancerous lymph nodes and an enlarged spleen. Cancerous lymphocytes can also form lymphoma tumors in places in the body outside of the lymphatic system. This is because lymphocytes can also travel in the bloodstream.
Who gets non-Hodgkin’s Lymphoma?
Anyone can be affected. Most cases occur in people over the age of 60. Men are more commonly affected than women.
Who gets Hodgkin’s Lymphoma?
Anyone can be affected, including children. However, most cases occur between the ages of 20 and 25 years, or after the age of 70. It is one of the few cancers where there is a peak of incidence in young adults.
What are the signs & symptoms of Lymphoma?
Enlarged Lymph Nodes: The most common early symptom is to develop one or more swollen lymph nodes in one area of the body – most commonly the side of the neck, and armpit, or the groin. The swollen lymph nodes tend to be painless and gradually get bigger. If the affected lymph nodes are in the chest or abdomen, you will not be aware of the swelling in the early stages of the disease.
However, the most common cause of swollen lymph nodes is infection. Lymphoma may be suspected if lymph nodes remain swollen, or if there is no infection to cause the swelling.
Various other general symptoms may also develop, e.g.:
- Recurrent fevers (greater than 38ËšC)
- Night sweats (drenching)
- Weight loss (greater than 10% in less than six months)
- Fatigue (severe and persistent)
As a lymphoma develops you may feel generally unwell. If the lymphoma tumors become large and press on nearby parts of the body, various other symptoms can develop. For example, you may develop a cough or breathing problems if the tumor enlarges in the lymph nodes inside the chest, stomach pain if the lymphoma develops in the stomach.
How is Lymphoma diagnosed?
Lymphoma is generally diagnosed on a biopsy of enlarged lymph nodes. A biopsy is when a small sample of tissue is removed from a part of these nodes. Sometimes an entire lymph node is removed. The sample is then viewed under a microscope to look for abnormal cells, patterns, and grade of lymphoma. In Hodgkin’s lymphoma, a cell called the Reed-Sternberg cell is seen under a microscope.
An additional test like immunohistochemistry (IHC) is performed for identifying subtypes of lymphoma. In some cases, this sample may be processed for cytogenetics or immunophenotype.
What are the different types of non-Hodgkin’s Lymphoma?
Non-Hodgkin’s lymphoma is also divided as High-Grade (fast-growing) or Low-Grade (slow-growing) depending on grade and B cell or T cell depending upon cell of origin. The common types of non-Hodgkin’s lymphomas include diffuse large B-cell lymphoma, lymphoblastic lymphoma, follicular lymphoma, anaplastic large-cell lymphoma, lymphoplasmacytic lymphoma, and mantle cell lymphoma – but there are various other types. Different types of lymphoma are treated differently and a different outlook.
What are the different types of Hodgkin’s Lymphoma?
There are various sub-types of Hodgkin’s lymphoma. It is divided into classical Hodgkin’s lymphoma and lymphocyte-predominant Hodgkin’s lymphoma as treatment of these two types different.
How is Lymphoma staging done?
The aim of staging is to find out how much the lymphoma has grown locally, and whether it has spread to other lymph nodes or to other parts of the body. For determining the stage of lymphoma CT scan, blood tests, a bone marrow biopsy, or other tests are performed. Nowadays PET/CT scans are considered superior to CT scans and preferred. All staging investigations are repeated at end of treatment for documenting complete clearance of lymphoma. PET scan can be done in the interim after 2-3 cycles of chemotherapy for assessing initial response to chemotherapy.
Ann Arbor staging of Lymphoma
- Stage 1: The lymphoma is confined to one group of lymph nodes only.
- Stage 2: The lymphoma affects two or more groups of lymph nodes. However, they are all on the same side of the diaphragm. (The diaphragm is the large muscle that separates the chest from the abdomen and helps us to breathe. So, for stage 2, all the affected nodes will either be above or below the diaphragm.)
- Stage 3: The lymphoma affects nodes on both sides of the diaphragm.
- Stage 4: The lymphoma affects parts of the body outside of the lymphatic system.
Each stage is also divided into A or B. ‘A’ means that you do not have symptoms of night sweats fevers or weight loss. ‘B’ means that you do have one or more of these symptoms.
Medical Oncology
Medical Oncology is one of the three pillars of cancer treatment along with surgery and radiotherapy. It deals with the treatment of cancer using drugs that kill cancer cells. The aims of the treatment include cure, prolongation of life, relief of symptoms, and providing good quality of life, depending on the extent of disease at presentation. Recent years have seen the advent of several new chemotherapy drugs and also targeted therapy to help achieve the above-mentioned aims.
Medical Oncology involves treating cancer using the following drugs:
- Chemotherapy: These are drugs that kill cancer cells or stop their growth. However, they also act on normal body cells, thus leading to side effects.
- Targeted Therapy: These drugs target cancer cells specifically, sparing normal cells, thus limiting side effects.
- Hormonal Therapy: This involves the use of hormonal agents for the prevention and treatment of certain cancers such as breast cancer and prostate cancer.
.jpg) Chemotherapy Day Care Unit
Chemotherapy Day Care Unit
We have a dedicated daycare unit for patients receiving outpatient chemotherapy. This is manned by our chemotherapy specialist nurses. Apart from giving chemotherapy and targeted therapy, we also administer supportive treatment like blood transfusion, platelet transfusion, growth factor support, and intravenous fluids in the daycare unit. It has a procedure room for performing routine medical procedures such as lumbar puncture, pleural fluid drainage, ascitic fluid drainage, bone marrow aspiration, and biopsy. There is a separate pharmacy room for proper handling and preparation of chemotherapy drugs. The daycare unit is equipped with a cable television facility for entertainment during chemotherapy administration.
Why AIMS
The department has been set up with an aim to provide state-of-the-art, safe and effective treatment in a clean environment. We plan to target all aspects of the patient illness with a multi-disciplinary approach involving a team of medical oncologists, surgical oncologists, radiation oncologists,s and support services like preventive oncology, palliative care clinic, counseling, and rehabilitation. Chemotherapy and targeted therapy are provided, both, in inpatient and outpatient facilities.
Facilities
- 10 beds chemotherapy daycare unit located on the 4th floor.
- Chemotherapy specialist nurses trained in the administration and monitoring of chemotherapy.
- Counselors to deal with the psychosocial aspects of cancer.
- Specialists in giving supportive care to terminally ill cancer patients.
Pediatric Cancer
Pediatric (childhood) cancers are different from adult cancers as there are no clear causative factors as to why a child gets cancer. The most common childhood cancers are leukemia, lymphoma, and brain cancer.
Cancer in children is certainly distressing but here is a reason to smile-pediatric cancers tend to respond better to treatment, compared to adults. Children can usually be cured for life. It is essential to be patient and trust your doctor.
Warning signs
- Unexplained weight loss
- Headaches, often with early morning vomiting
- Pain/swelling in bones, joints, back, or legs
- Lump or mass in the abdomen, neck, chest, pelvis, or armpits
- Excessive bruising, bleeding, or rash
- Constant infections
- A whitish color behind the pupil
- Persisting nausea
- Constant tiredness or noticeable paleness
- Eye or vision changes that occur suddenly and persist
- Recurrent fevers of unknown origin
Risk factors
- Longer life expectancy in children allows a longer time for cancer processes to manifest, increasing the risk of developing some cancer types later in life.
- Genetic and familial factors are identified in 5-15 percent of pediatric cancer cases.
- Environmental exposure such as prenatal exposure to tobacco, X-rays, or certain medications is identified in <5 percent of cases.
- For the remaining 95 percent of cases, however, individual causes remain unknown
Progression
Different types of cancers in children spread to different organs of the child’s body. Leukemia may affect the brain and spinal cord, testicles, rarely ovaries, kidneys, and other organs. Lymphoma may spread to the liver, bone marrow, or spleen. Brain tumors may spread to spinal cord tissue. Rhabdomyosarcoma, when it spreads, creates new lesions in the lymph nodes, bone, bone marrow, or lung.
Diagnosis
- Primary diagnosis: Physical examination, blood tests
- Advanced diagnosis: Biopsy, bone marrow aspiration and biopsy, lumbar puncture, ultrasound, computed tomography scan (CT or CAT), magnetic resonance imaging (MRI), and positron emission tomography (PET) scan may be performed.
Pancreatic Cancer
The pancreas is a gland about 6 inches long, shaped like a thin pear. It lies between the stomach and the spine. It has two main jobs in the body—to make juices that help digest (break down) food and to make hormones, such as insulin and glucagon, that help control blood sugar levels. Pancreatic cancer is a disease in which malignant (cancer) cells form in the tissues of the pancreas.
Warning signs
- Jaundice (yellowing of the skin and whites of the eyes)
- Light-colored stools
- Dark urine
- Pain in the upper or middle abdomen and back
- Weight loss for no known reason
- Loss of appetite
- Feeling very tired
Some other symptoms are abdominal pain, back pain, fever with chills, and vomiting.
Risk factors
- Smoking
- Being overweight
- Old Age
- Having a personal history of diabetes or chronic pancreatitis
- Having a family history of pancreatic cancer or pancreatitis
- Having certain hereditary conditions, such as multiple endocrine neoplasia type 1 (MEN1) syndrome, hereditary non-polyposis colon cancer, hereditary breast, and ovarian cancer syndrome, familial atypical multiple mole melanoma (FAMMM) syndromes
Progression
- Stage I: The tumor is in the pancreas, has not spread to lymph nodes or other parts of the body
- Stage II: The tumor extends beyond the pancreas, but has not spread to nearby arteries, veins, lymph nodes, or other parts of the body
- Stage III: The tumor has spread to nearby arteries, veins, and/or lymph nodes but has not spread to other parts of the body
- Stage IV: Tumor has spread to other parts of the body (liver, peritoneum, lungs) It can spread to adjuvant organ-like small bowel, vessels, liver, lungs and give rise to jaundice and mass abdomen, back pain, and vomiting.
Diagnosis
- Primary diagnosis Physical exam and history, blood chemistry studies, tumor marker tests
- Advanced diagnosis MRI, CT scan, and PET scan, abdominal ultrasound, endoscopic ultrasound, laparoscopy, and biopsy (not mandatory).
Prostate Cancer
Prostate Cancer is a disease that only affects men. Cancer begins to grow in the prostate, a gland in the male reproductive system.
Prostate cancer is now the most commonly diagnosed male cancer in many Western countries and records show that its incidence is increasing in India. The number of recorded cases has increased a lot in recent years. This is partly due to the increased use of the Prostate-Specific Antigen (PSA) test, which has resulted in more cases being detected and partly due to the fact that men are living longer. Like most cancers, prostate cancer is more common in those over 60. In 2013, more than 242,000 men will be diagnosed with prostate cancer, and more than 28,000 men will die from the disease. One new case occurs every 2.1 minutes and a man dies from prostate cancer every 18.6 minutes.
Particularly in Asia, we face a future major increase in the rates of prostate cancer. Collaborative action now is a high priority to allow the preparations necessary for effective control of prostate cancer.
What is Prostate Cancer?
Prostate cancer is caused when cells in the prostate multiply and grow out of control to form a mass or tumor. Being a very variable disease, some tumors remain small and grow so slowly that they cause no problems for the rest of a man’s life; others are aggressive (which may eventually spread to the bone), grow quickly, and become life-threatening.
Why one needs to be aware?
If prostate cancer is diagnosed early (before it has spread outside the prostate gland) it can be treated very successfully. The treatment provides a long-term cure for at least 9/10 cases. However, when the cancer is advanced, it becomes very difficult to cure. If cancer has spread outside the gland, the prospects are worse. Even a small amount of spread reduces the chance of a cure. A more distant spread makes a cure very unlikely. Treatment can give these patients extra years of life and stop the pain of the disease but is only able to cure a minority of them. Overall, only about one in three of patients with cancer spread outside the prostate survive for five or more years after the diagnosis. All men over 50 should be aware of the warning signs and check with their doctor at regular intervals.
What are the common signs and symptoms?
Early-stage prostate cancer does not cause any symptoms. So men who are above 50 years of age are advised to undergo voluntarily testing for prostate cancer.
Warning signs
- Frequent urination, more often at night
- Difficulty in urinating
- Blood in the urine / painful urination
- Ejaculation may be painful (less common)
- Achieving or maintaining an erection may be difficult (less common).
- Inability to urinate
- Passing urine often (particularly at night)
- Weak or interrupted urine flow
- Pain when urinating
- Pain in the lower back, hips, and upper thighs
However, all of these symptoms can also be caused by other conditions, such as benign prostate enlargement. Men with any of these symptoms should consult their doctor.
Sarcomas (Bone Cancer)
Primary bone cancer (Bone Sarcomas), which begins in the bone is rare cancer. Bone cancer can begin in any bone in the body, but it most commonly affects the long bones in the arms and legs.
More commonly we encounter metastatic bone cancer, which is a cancer of other organs that has spread to the bone.
Warning signs
- Bone pain
- Swelling and tenderness near the joint
- Difficulty in normal movements
- Broken bone
- Fatigue
- Unintended weight loss
Risk factors
Most of the patients who develop bone cancer do not have any risk factors. However, certain factors are associated with an increased risk, including:
- Inherited genetic syndromes like Li-Fraumeni syndrome and Hereditary Retinoblastoma
- Paget’s disease of bone that occurs mostly in older adults
- Exposure to large doses of radiation, such as those given during radiation therapy for cancer, increases the risk of bone cancer in the future
Progression
- Stage I: The tumor is low grade, has not spread to any lymph nodes or to other parts of the body.
- Stage II: The tumor is high grade but has not spread to any lymph nodes or to other parts of the body.
- Stage III: Multiple tumors in the primary bone site, but they have not spread to any lymph nodes or to other parts of the body.
- Stage IV: Tumors have spread to the lung(s) and/or other organs besides the lungs
Diagnosis
- Primary diagnosis: Medical history, Physical examination
- Secondary diagnosis: Imaging tests like radiographs, MRI and/or CT scan, Biopsy (sample of tissue from the tumor)
- Advanced diagnosis: Bone scan, PET scan, CT scan of the chest, etc.
Stomach Cancer
Nearly everyone has had a stomachache at some point due to different reasons. It generally isn’t taken seriously because it’s quite common. But, on certain occasions, a stomach ache can be indicative of a far more serious problem – digestive tract complications, colitis, and even cancer. Tackling these conditions at an early stage ensures you a better chance of survival. In cases involving colonic cancer and colitis, timely intervention can save the lives of 70-80per cent of patients. So, make it a point to visit your doctor regularly for check-ups.
Warning signs
- Poor appetite
- Weight loss (without trying)
- Abdominal (belly) pain, discomfort
- A sense of fullness in the upper abdomen after eating a small meal
- Heartburn or indigestion
- Nausea vomiting, with or without blood
- Swelling or fluid build-up in the abdomen
- Low red blood cell count (anemia)
Risk factors
- A diet high in salty and smoked foods
- A diet low in fruits and vegetables
- Smoking
- Eating foods contaminated with aflatoxin fungus
- Family history of stomach cancer
- Infection with Helicobacter pylori (a type of bacteria)
- Long-term stomach inflammation
- Pernicious anemia
- Stomach polyps
Progression
- Stage I: Cancer has grown into the inner layer of the wall of the stomach
- Stage II: Cancer has grown into the outer muscular layers of the wall of the stomach
- Stage III: Cancer has grown through all of the layers of the muscle into the connective tissue outside the stomach and has grown to nearby organs or structures
- Stage IV: Cancer has spread to the liver and to the inside of the abdomen. Less commonly, it can also spread to the lungs.
Diagnosis
- Primary diagnosis: Physical examination
- Advanced diagnosis: Biopsy, endoscopy, endoscopic ultrasound, X-ray, barium swallow, computed tomography (CT or CAT) scan, magnetic resonance imaging (MRI), positron emission tomography (PET) scan, laparoscopy.
Urinary Bladder Cancer
Urinary Bladder Cancer begins when cells in the urinary bladder start to grow uncontrollably.
The bladder is a hollow organ in the lower abdomen (pelvis), which collects and stores urine produced by the kidneys. It is estimated that there are 383,000 cases of bladder cancer worldwide out of which they are most commonly found in industrialized countries. Bladder cancer occurs mostly among older individuals although it has been noted to appear among the younger age groups as well. The average age of diagnosis is in the 60s. Cancer has a high rate of recurrence.
What is cancer of the bladder?
Bladder cancer is a type of malignancy arising from the epithelial lining (i.e., the urothelium) of the urinary bladder. It is a disease in which abnormal cells multiply without control in the bladder. The most common type of bladder cancer recapitulates the normal histology of the urothelium and is known as transitional cell carcinoma or more properly urothelial cell carcinoma.
What are the common signs and symptoms?
Early-stage tumors may not give any symptoms. Common symptoms of bladder cancer include:
- Blood in the urine
- Pain or burning during urination
- Feeling as if you need to go right away, even when the bladder is not full
- Having trouble urinating or having a weak urine stream
- Frequent urination or feeling the need to urinate without results
- Pain or burning during urination
These symptoms are not sure signs of bladder cancer. Infections, benign tumors, bladder stones, or other problems also can cause these symptoms. Anyone with these symptoms should see a doctor so that the doctor can diagnose and treat any problem as early as possible. If there is blood in the urine, then one should be careful and should not neglect it.
Specialists
.jpg)
DR. SUPRIYA BAMBARKAR
DIRECTOR (DEPT. OF ONCOLOGY), CONSULTANT ONCOSURGEON
D.N.B., M.Ch. (Surgical Oncology)
View details
Appointment

DR. RAKESH PATIL
MEDICAL & HEMATO ONCOLOGIST
M.D. (Medicine), D.M. (Medical Oncology and Hematology)
View details
Appointment

MR. CHANGDEV TAHAKIK
CHIEF MEDICAL PHYSICIST & RADIOLOGICAL SAFETY OFFICER
M.Sc. (Phy), Dip. R.P. (B.A.R.C)
View details
Appointment
ABOUT US
About AIMSDirector's Message
Vision & Mission
Accreditations
Awards & Accolades
Our Network
Phone Directory
Designed by Web Creations 2022. All rights reserved.






.jpg)